health law and policy assignment assessing Euthanasia legalities
Question
Task: Can health law and policy assignment reaserch strategies be implemented to justify Euthanasia laws?
Answer
Introduction
As per health law and policy assignment reports, Euthanasia is the act of assisting terminal ill people in having death without any suffering with the help of doctors and health professionals. It advocates for people to have peaceful death without any suffering, and it has allowed patients to die with the help of doctors who are on the verge of death. The End of Life Choice Act was effective in 2019 after it was voted by the public in general regarding euthanasia. The act will be regulated if the person is terminally ill and their life is for six to seven months. The act will be regulated with the consent of the patient and won't be legal if it is implemented on mentally ill or retarded people.Many people also protested the act or issue as this can decrease humanity and social well-being. The medical science in bringing innovation in a cure for the disease might lack in bringing effectiveness. The alternative solution for euthanasia concerning terminal ill death in palliative care, where patients get proper medication and have peaceful death without any suffering.
Analysis of dilemma
The chosen health law and policy assignmentcase study is the Euthanasia referendum, which was held on 17th October 2020 in New Zealand, where the voting process started on 3rd October. The main concept of the euthanasia referendum was to pass and make use of the End of Life Choice Act 2019 within the country and its healthcare system. A long voting process was conducted in union with the 2020 general election and Cannabis referendum to make the act forceful within the country. It has been found that New Zealanders successfully voted to the respective legalise euthanasia for people suffering from a terminal illness. The result that was announced later by the electoral commission demonstrates that about 65.2% of people agreed with the decision to do the act in force, whereas 33.8% of the people refused it considerably (Roy, 2020).
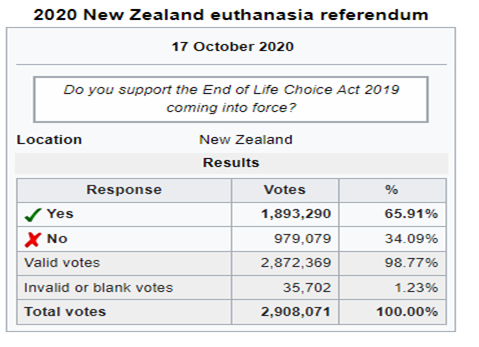
Figure 1: Euthanasia referendum in New Zealand
Source: (Roy, 2020).
Moreover, as demonstrated in the above image, the majority of the voters supported the legislation, and the bill came to force from 7th November 2021, one year after the final result. It was reported that euthanasia was an act of illegal aspects in New Zealand, and under section 179 of the New Zealand Crime Act 1961, euthanasia encourages suicide among people with a terminal illness (Ministry of Justice, 2014). Two attempts to legalise euthanasia already failed in the parliament of New Zealand; however, it was passed finally in 2020. The dilemma was to choose between the two viable options
Yes, I support the End of Life Choice Act 2019 coming into force
No, I do not support the End of Life Choice Act 2019 coming into force.
The health law and policy assignmentdilemma, as stated above, was very difficult to choose between one since it was a decision to be made that could influence the entire health care sector of New Zealand. Although the choices were made within acertain period of time, and it came into force in November 2021, it has been found that at least 32 people in New Zealand have taken the service after euthanasia became legal in the country (McClure, 2022). The act, as mentioned earlier, gives specific people a legal consideration to ask for medical assistance to bring their life to an end if they have been suffering from a certain terminal illness. The act was passed in the year 2019 and was waiting for at least a 50% vote in the next upcoming year, 2020; it appears to be successful, and now the act is in force in New Zealand.
According to Gill (2020), the act of assisted suicide in New Zealand came into excessive account after a lawyer, Lecretia Seals, cased a file for an assisted death when she was diagnosed with brain cancer. The treatment that she was getting was at an extreme level which was not bearable, and she wanted to have an assisted death. Lecretia Seals, with her lawyer, cased a file to the high court of New Zealand seeking assisted death. However, she did not get any such permission from the court; however, the case of Lecretia Seals greatly impacted the further referendum on euthanasia in 2020 (Vickers, 2020). The act that has been passed considers a legal assisted death to the patient suffering from a terminal illness and to those who have less than six months of their life. It is a deliberate act of ending someone's life and making them free from certain pain or illness. However, such acts cannot be found in force in other countries and are still considered illegal acts by the government. It is observed on this health law and policy assignmentthat after five years of Lecretia Seals's death, New Zealanders got an opportunity to vote for and against the legislation related to voluntary euthanasia (Meng-Yee, 2020). The legislation now can be found active in New Zealand, and individuals and families seem to be happy for those suffering from a terminal illness.
Alternatives and decision criteria
In New Zealand, the "End of Life Choice Act 2019" was regulated related to the health disease above the age of 18 who are terminally ill and are going to live for a maximum of six to seven months. The vote was going in general public with two referendums, the end of life choice and cannabis referendum, where voters rejected the cannabis referendum. The act emerged in New Zealand when female lawyer Lecretia Seale saws diagnosed with brain cancer in 201, and there was not any further treatment concerning the disease. The lawyer wanted to end her life with the help of her physician. For legalising medical death, if the person is terminal ill and wants to end her life with the help of a physician and doctor, it has to be allowed. The vote regarding this was announced to make this an act. Therefore, in 2019 the vote was in favour of the legalisation of the act. However, there were many people who opposed the act. The act defends to implementation of this law if the person is mentally ill or is suffering from a mental disorder (Gill, 2020).
There were certain people gathering to march and protest against the legalisation of the "End of Life Choice Act 2019" in the country. The protestors gathered in Christ's church against euthanasia rejection, and more than 1000 people participated in the rally. The spokesperson of the Right to live group Ken Orr said that the beauty and dignity of human life need to be protected and valued in the country for a better purpose (Guildford, 2020). In New Zealand, many doctors also came in front in favour of dismissing and rejecting euthanasia in the country. Dr Donnelly, who is one of the doctors who opposed the act among 1500 doctors, wrote an open letter to the parliament stating to dismiss the bill on euthanasia. The doctor stated that doctors are meant to save the lives of people by providing proper care and treatment, and there is no place for ending the lives of people intentionally. Dr Donnelly also added that they stand with the world medical association, that is, in 114 countries, in favour of dismissing the act and in not ending the lives of people intentionally (Roman Catholic Archbishop, 2019).
As per research done on this health law and policy assignment, the catholic denominations stated that in euthanasia, it is more unethical and dangerous for people to assist doctors in having a peaceful death without any suffering, which could be said as suicide. Palliative care provided to terminally ill people so they can die peacefully is dangerous as this can lack the effectiveness of safeguarding people and especially who are willing to die a peaceful death. As per the catholic, people who are terminally ill should be provided proper care, affection, attention, and supporting them in their difficult times (Reis, 2020). Encouraging euthanasia in New Zealand can lack the interest in bringing innovation in medical science and finding new cure treatments. The people who are terminally and do not want to regulate euthanasia may get pressurised by their family members and relatives, and this lacks humanity massively. The regulation of euthanasia or the "end of life by choice act" could reduce the humanity, love and care in the society, and this can also lack the value of human life. The care, treatment, and love the patient wants to get from their relatives might get reduced (BBC, 2022).
An alternative solution identified on this health law and policy assignment is the treatment of a terminal ill person are to provide hospice and proper treatment with care and love. If the person is terminally ill with no solution to cure their disease and is living on the verge of death as per the doctors' suggestion, it is imperative to provide palliative care or hospice to them. Palliative care provides treatment to them in accepting the fact death is a natural process to end life. In this care, the doctors or health professionals provide medications that help in relieving pain and suffering from the disease, and a person can have a peaceful death. The main purpose of palliative care is to provide medication to terminal ill patients, so they can die without suffering and with dignity. Palliative care is mostly provided to people who are suffering from cancer or untreatable disease. However, palliative care is falsely presented in medical care to cure disease or provide comfort care (Erdek, 2015). Therefore, the alternative solution to terminal ill-treatment is hospice or palliative care.
Proposed solution with justification
As identified earlier, some people voted against voluntary euthanasia and protested against it and were not ready to make the government an active legislative to come into force. It is because of the different choices and perspectives of the people who appear to be different from one person to another. It can be said that the choices depend on the person to take voluntary euthanasia or to go with another option since no one can be forced to their choices. Nonetheless, the options can be found as mentioned above, and the proposed solution for euthanasia is hospice care which is considered one of the appreciated alternatives for euthanasia. Wajid et al. (2021) stated that hospice is an approach that counts people belonging to various disciplines and provides them with comprehensive care for those near death and about to end their life.Hospice care can be provided to patients in theterminal phase and consists of fewer than six months of life expectancy. It is because hospice care depends on a person's life expectancy, which is crucial for their overall care.Hospice care can be seen as an appealing solution compared to voluntary death because involuntary death, there might be certain issues that could hamper the patient's life.
Furthermore, as identified on this health law and policy assignment, as an alternative solution for euthanasia, a hospice care solution has been appreciated by most people in the past few decades because of the argument developed by voluntary euthanasia associated with health care (Cohen-Almagor, 2015). Hospice care solutions for terminal illnesses will keep the health care approach alive without any negligence from the respective individual and organisation. The solution of hospice care is suggested because, through this approach, the world of science can remain innovative and try to make a difference within the health care sector and bring specific solutions for such terminal illnesses. As known to everyone that within the health care sector, the care of the patient is very crucial. If the option of voluntary euthanasia is available, the care may get neglected by the health professionals. According to Noe (2017), voluntary euthanasia devalues the life of a people, and many religious scholars have argued it is an immoral act by humans. Therefore, to not devalue any human and not degrade the health care practice, the solution of hospice care needs to be adopted by the healthcare sector as an alternative to voluntary euthanasia (Banovic & Turanjanin, 2014).
Recommendation
A person suffering from a terminal illness and no option left can be helped with hospice care as mentioned above, however, with certain strategies. As per Oliver et al. (2016), the caregivers can focus on three subsequent areas as a strategy to implement hospice care as an alternative. These three strategies are as follows:
Patient care strategy: This strategy is based on the issue that the patient is suffering from. It ensures the respective patients get adequate care within a safe environment when they are challenged alone.
Self-care strategy: This strategy can be implemented based on emotion and issues and considering the past caregiving experiences (Oliver et al., 2016). Here the patient can be encouraged with positive talk, social time, work, physical activities etc.
Emotional support strategy: The caregiver needs to continuously communicate with the patient's family through this strategy. Friends, family, and colleagues can support this strategy and make a patient feel better in such a harsh time. It is the most appreciated strategy to be implemented during euthanasia which will support a positive environment and better care for the patient.
Conclusion
On this health law and policy assignmentEuthanasia is one of the current topics that are highly discussed in New Zealand. It came to light when a person suffering from a brain tumour assisted her physician to have provided a sedative for her death. In 2019 the government of New Zealand regulated the act "End of Life Choice 2019", which was done with the consent of the general people by doing voting system in the country. However, various people, i.e. doctors, catholic people, and NGOs, opposed the regulation of the act as it could decrease the effectiveness of medical science in finding treatment to cure disease and humanity and love in the society. The main reason for opposing euthanasia in New Zealand was that it could decrease the human affection, love and humanity in the society. The doctors who were protesting the act also defined that doctors aremade for saving the lives of people and providing proper care to them rather than taking the lives of people intentionally.The alternative solution observed on this health law and policy assignment isprovided by doctors for terminally ill people are hospice or palliative care which helps in reducing pain and having a peaceful death with dignity.
References
Banovi, B., & Turanjanin, V. (2014). Euthanasia: Murder or Not: A Comparative Approach. Iranian Journal of Public
Health, health law and policy assignment43(10), 1316–1323. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4441884/
BBC. (2022). Euthanasia - Revision 3 - GCSE Religious Studies - BBC Bitesize. BBC Bitesize; BBC. https://www.bbc.co.uk/bitesize/guides/zynv87h/revision/3
Cohen-Almagor, R. (2015). (PDF) An argument for physician-assisted suicide and against euthanasia. ResearchGate. https://www.researchgate.net/publication/284246278_An_argument_for_physician-assisted_suicide_and_against_euthanasia
Erdek, M. (2015). Pain Medicine and Palliative Care as an Alternative to Euthanasia in End-of-Life Cancer Care. The Linacre Quarterly, 82(2), 128–134. https://doi.org/10.1179/2050854915y.0000000003 Gill, M. (2020, 3rd November). Explained: What is New Zealand’s euthanasia or assisted dying act? The Indian Express. https://indianexpress.com/article/explained/explained-what-is-new-zealands-euthanasia-or-assisted-dying-act6910183/ Guildford, J. (2020, 16th August). Protesters in Christchurch march against euthanasia referendum. Stuff. https://www.stuff.co.nz/national/health/euthanasia-debate/122462731/protesters-in-christchurch-march-against-euthanasia-referendum
McClure, T. (2022, 9th February). At least 32 people take advantage of New Zealand assisted dying laws in first three months. The Guardian. https://www.theguardian.com/world/2022/feb/08/at-least-28-people-take-advantage-of-new-zealand-assisted-dying-laws-in-first-three-months
Meng-Yee, C. (2020). “You have our permission to go”: Lecretia Seales’ parents on euthanasia. NZ Herald. https://www.nzherald.co.nz/nz/lecretia-seales-parents-on-voluntary-euthanasia-and-her-legacy/WIJAP745W36X67MEZPIX6DFMLI/
Ministry of Justice. (2014). Crimes Act 1961. https://sherloc.unodc.org/cld/uploads/res/document/nzl/1962/crimes_act_1961_html/New_Zealand_
Crimes_Act.pdf
Noe, S. M. (2017). Euthanasia; Letting die. ResearchGate. https://www.researchgate.net/publication/330185818_Euthanasia_Letting_die
Oliver, D. P., Demiris, G., Washington, K. T., Clark, C., & Thomas-Jones, D. (2016). Challenges and Strategies for Hospice Caregivers: A Qualitative Analysis. The Gerontologist, gnw054. https://doi.org/10.1093/geront/gnw054
Reis, B. M. (2020, 29th September). New Zealand church leaders on End of Life Choice Act - Vatican News. Www.vaticannews.va. https://www.vaticannews.va/en/church/news/2020-09/new-zealand-euthanasia-referendum-end-of-life-choice-church.html
Roman Catholic Archbishop. (2019, 28th November). Protestors say “No” to Euthanasia Bill | Archdiocese of Wellington.health law and policy assignment Www.wn.catholic.org.nz/. https://www.wn.catholic.org.nz/adw_welcom/protestors-say-no-to-euthanasia-bill/ Roy, E. A. (2020, 30th October). New Zealand votes to legalise euthanasia in referendum. The Guardian. https://www.theguardian.com/world/2020/oct/30/new-zealand-votes-to-legalise-euthanasia-but-against-legalising-cannabis-in-referendum
Vickers, M. (2020, 3rd November). My late wife, an extraordinary hero, was instrumental in New Zealand legalising assisted dying | Matt Vickers. The Guardian. https://www.theguardian.com/commentisfree/2020/nov/03/my-late-wife-an-extraordinary-hero-was-instrumental-in-new-zealand-legalising-assisted-dying Wajid, M., R, E., John, R. john, & George, A. J. (2021). Why is hospice care important? An exploration of its benefits for patients with terminal cancer. ResearchGate. health law and policy assignmenthttps://www.researchgate.net/publication/351649276_Why_is_hospice_care_important_An _exploration_of_its_benefits_for_patients_with_terminal_cancer,