Nursing Assignment: Health Needs of Individuals with Type 2 Diabetes in Leicester City
Question
Task: Prepare a well researched and detailed nursing assignment critically analysing the health needs of individuals with Type 2 Diabetes in the city of Leiceter.
Answer
Abstract
This report on nursing assignment is prepared to look at the “city of Leicester” regarding “Type 2 Diabetes (T2D)” in people as well as the existence of diabetes in Leicester city. It will also consider the demographic as well as the epidemiological profiles of “city of Leicester” and comparing it to that of England. Moreover, the influence of the rates of T2D in association with factors like age, ethnicity, deficiency, and existence of obesity and unemployment has been discussed. A comparison has been made between Leicester and England linking these aspects.
The report will identify the community services in the “city of Leicester” for the population with T2D. Then the identified community services in the region includethe“Integrated Community Diabetes Service (ICDS)” along with the “Diabetes Education and Self-management for Ongoing and Newly Diagnosed (DESMOND)”. It has been detected that the gaps along with the inequalities areexistingservices available currently for T2D in Leicester. It has been sketched that individuals belonging to BME backgrounds and vulnerable groups are poorly aided.
The current scope of analysis has considered working from a multi-agency that includes the responsibility of the statutory body, voluntary agencies, as well as the carer/family. The analysis hascriticallyassessedand evaluated the “health needs (HN)” of individuals residing in the “city of Leicester” with T2D. The report has constructed with HN assessment applying the “Maslow’s Hierarchy of Needs (HON)” evaluating criticallythe physiological, belongingness, safety, “self-esteem”, and finally “self-actualization” needs of the patients. The report has explained how the LD nurse can help in empowering patients.
1.0 Introduction
The features of age, deficiency, ethnicity, along with prevalence for the "city of Leicester and England” will be observedas well as compared between Leicester and England. “Community services for T2D” in the "City of Leicester”has beenrecognizedalongside the gaps as well as existing inequalities in the service delivery. The HN of T2D patients will be measured and critically examined using “Maslow’s Hierarchy of needs”. The current scope of analysis will discover a nurse’s role along with specific intervention strategies applied by nurses for patients detected with “T2D”. Confidentiality will be maintained in this report as per the NMC Code of Conduct (2016).
Health is seen impacted by several factors, which includes:-
• “Physical environment”
• “Social environment – family/friends or norms and values”
• “Economic compensations/ poverty”
• “Behaviour and lifestyle –an unhealthy diet can lead to obesity and type 2 diabetes”
• “Family genetics and individual”
2.0. T2D Diabetes definition
According to Tripathy et al (2010) “Type 2 Diabetes” as a general condition of health, that includes a predisposition of geneticsinthegradualloss of beta-cell mass as well as the function of insulin resistance”. The various underlying environmental factors of“type 2 diabetes” like obesity, low physical exercise, high rates of alcohol consumption, along with poor dietary habits are seen to have a connectedness to “T2D”. Several patients with diabetes are seen to have existing co-morbidities that include “heart failure”, “hypertension”, and “kidney failure”. The treatment for “type 2 diabetes” currentlyestimates at approximately amounting to 9% of the total NHS budget (NHS, 2020).
2.1 Prevalence
Approximately 3.7 million population in the UK are detected with diabetes while it is also estimated to be at five million by 2025while T2D comprises 90% of this figure (DUK, 2012). In England, diabetes is a major reason for premature mortality and approximately 23,300 deaths from 2010 to 2011 were attributes of diabetic patients (PHE, 2014). At present, the prevalence of T2D in Leicester is 9.7% and if this trend continues, the prevalence is estimated to hit 13% in 2030 (NDIS, 2015).
3.0. Demographic profile
3.1Introduction
Epidemiology is referred to as the study of the cause of disease thereby usingtheresults for evaluating approaches to prevent diseases (World Health Organisation 2017). In this view, Leicester’s population currently is seen to be at 330 000 whichcan be anticipated to become 345 000 by 2021.
3.2“Age & Gender”
It is pertinent to evaluate the distribution of age prevalent in the community as it majorly influencesthe health needs. It has been observed that the younger as well as elderly peoplepossessdiverse health needs. However, amongst the vast majority of “T2D” patients’ majorityare seen to be middle-aged.
Genes has also been considered a factor of “Type 2 Diabetes” thus if either of the parents is experiencing“Type 2 Diabetes” then it is likely that the child is at a 15% risk of developing T2D. However, in case bothparents are detected with“Type 2 Diabetes” then considerably the child isseen to be at a 75% risk of evolving diabetes. Men aged 65- 74 are at the highest risk of developing diabetes (Cities Changing Diabetes, 2018). Currently, 90% of adults aged 16-54 years are detected with “Type 2 Diabetes” have already existing conditions of obesity.
3.3 Education
There are only 3.9% are newly diagnosed for “type 2 diabetics” in the current year. They also have been provided with structured education for healthy eating. The “NHS trust” in the "city of Leicester” provides online sheets comprising of facts as well as defining of words that are generally applied in the healthcare settings during the treatment of type 2 diabetes. Moreover, the given information briefly explains treatment, risks, as well as benefits of such interventions (Cities Changing Diabetes, 2018). However, this leaflet is written in English which causes communication barrier other ethnic communities.
“City of Leicester”, is seen to have patient information along with educational leaflets for both that are existing patients with T2Das well as for the newly diagnosed patients diagnosed by the University Teaching Hospitals (UHL). These informational leaflets are made colourful, which are easy to read and apprehend. Such leaflets are developed to advise patients regarding where they can obtain leaflets in other languages. Such leaflets are made available in varied Asian language for matching the diverse demographic population present in Leicester.
3.4Ethnicity
Ethnicity and cultural background which has animportant impact on health, and individuals, “Leicester and Birmingham” is seen to have a diverse population. Black along with South Asian people are seen to be at higher risk from“type 2 diabetes”. The prevalence of T2D is strongly linked to ethnicity. It has been estimated 50% of the individuals in the "City of Leicester”belong from BME backgrounds are compared to England where the rate of prevalence is only 15%. A large part of the BME population residing in Leicester is a major of Asian origin. It can be said that Diabetes occurrence is very high in Asian communities. People from BME backgrounds are inactive than the general population, which further increases the risk factor for diabetes.
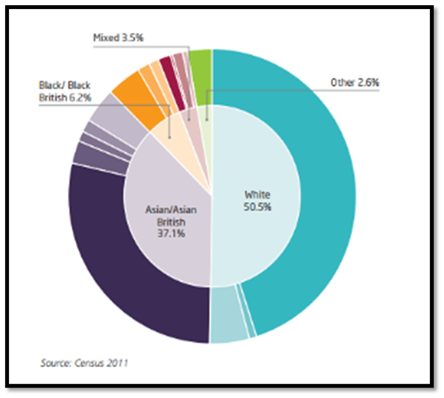
Figure 1:Ethnicityin Leicester
(Source: The British Diabetic Association, n.d)
However, black and Caucasian communities with similar incomes are also detected with Diabetes. People from Africa, Asia, as well as other ethnic minor groups are seen exposed to an equivalent risk of “Type 2 Diabetes” even at lower rates of BMI when compared against the white European population (Mostafa et al, 2012). In the general population, males (4.3%) are seen to have a greater prevalence of “Type 2 Diabetes”than women (3.3%). When such differences are noted amongst some ethnic minorities, such difference isseenhigher. For instance, amongst the Black African population “T2D” prevalence amongst men at 5% whereas it is at 2.1% when seen amongst women. Research depicts that in ethnic minorities such as Pakistani, such trend is reversed, as in women it is seen to be at 8.6% whereas amongst men it is at 7.3%. “T2D”has the highest prevalence amongst Indian men which is at 10.1%, while the ethnicity which shown the highest combined rate of prevalence includes the Black Caribbean with rates of T2D being 10% amongst men 10%, and 8.4% amongst women 8.4%. Religion as a factor was also seen to have an influence on a patient with “type 2 diabetes”. “Leicester”witha huge Muslim community was seen to have a higher prevalence of the T2D patient population (The British Diabetic Association, 2020). In Type 2 diabetics, individuals need to eat regularly for controlling their levels of blood sugar. For these cases, the “Diabetes Patient Education Programme (DESMOND)”has been made available for those newly diagnosed with diabetics in the "city of Leicester”.The “DESMONDprogram” is specifically for individuals with “T2D”, for them to assemble and discuss issues related to T2D.
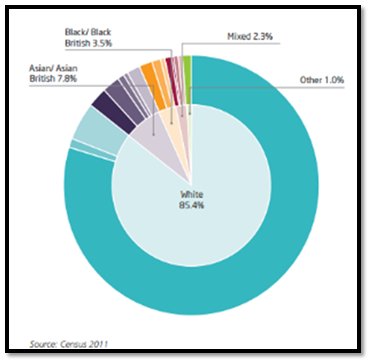
Figure 2Ethnicity in England
(Source: The British Diabetic Association, n.d)
4.0“Deprivation in England and Leicester”
The majority population within “Leicester city” is disadvantagedwhile some areas are seen to possess extreme as well as multiple levels of deprivation when compared with T2D prevalence. Leicester has been classified to be the 25th most underprivileged area out of 326 local authorities existing in England.
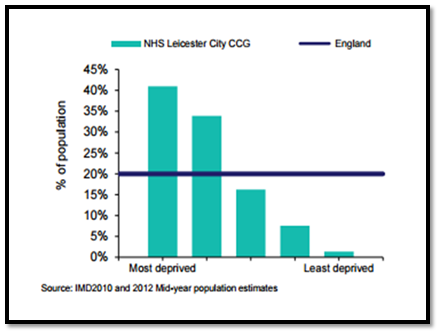
Figure 3:Population
(Source: Leicester City Council, 2015)
The prevalence of T2D is seen greater in communities which faces deprivation, as20% people in England are seen to reside in most deprived areas which poses 56% risk related to developing diabetes. Areas within Leicester are seen to fall in this category (NHS, 2017). The figure depicted below shows that 41% of the population in Leicester' is deprived when compared against 20% in rest of England. Due to low educational achievement levels is seen linked to deprivation whereas 44.2% of Leicester’s population not havingany qualifications, which considerably increases their risks of having T2D. The figure 4 depicts the areas in dark orange which is seen as the most deprived areas marked as 20%. Areas in the shaded orange areas are among the greatest deprived marked at 5% in England (LCC, 2014).
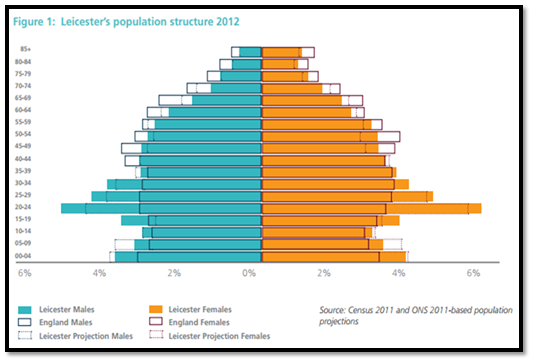
Figure 4: Leicester Population
(Source: Leicester City Council, 2015)
From figure 3, 41% of population of Leicester’s is deprived when compared against Englandamounting to 20%. Due to low prevalence of educational achievements which are directly linked to deprivation with 44.2% of Leicester population not havingadequatequalifications. Deprivation has been considered a risk factor connected to T2D. From the high rates of deprivation as prevalent in Leicester, currently the rate of “T2D” in “Leicester” is much greaterwhen compared to that of England.
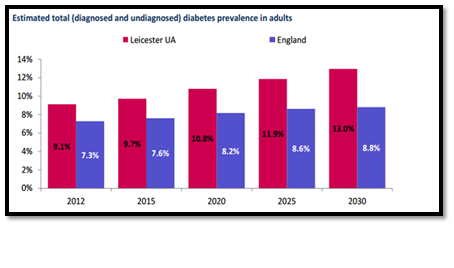
Figure 5:Diagnosed and Undiagnosed Population
(Source: Leicester City Council, 2015)
At present, the prevalence of T2D in Leicester is at 9.7% which when compared against England is at 7.6% which reveals significantly higher rates. In case the current trends continue, then the prevalence of T2D for “Leicester” is predicted to become 13% by 2030. As a result of prevalence of overall diabetes is considerably higher in “Leicester” due to varied factors which leads to higher levels of deprivation as well as large BME communities, who are all at considerable risk factors for diabetes.
Rate of prevalence of obesity in Leicester is at 19.6% that can be seen comparable to the whole of England at 23% (Leicester Government UK, 2015).It has been estimated that 71.0% of people in Leicester do not consume healthy meals that is not significantly distinct to that England at 71.3%. Leicester is seen to be at the bottom 25% who participates in sports with a mere 18% of the population who regularly exercises(WHO, 2016). Eating unhealthily as well as leading sedentary lifestyle have been considered as underlying risk factors for obesity for T2D in “Leicester and England”. Therefore, with risingoccurrencein obesity in “Leicester and England” has created an escalation in the occurrence of “T2D” in “Leicester and England”.Current rates of unemployment in Leicester is considerably higher when compared to that of England. Hence leading to higher rates of deprivation in Leicester, which in turn leads to T2D.All these analysis reveals that increase in prevalence of T2D for Leicester as unemployment is directly connected to deprivation which in turn possess as a risk factor for diabetes.
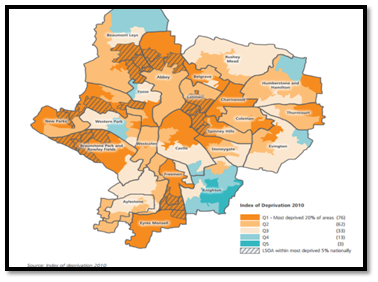
Figure 6- Deprivation in Leicester
(Source: Leicester City Council, 2015)
5.0 Community Services available
The ICDS is an MTD service that provides care for diabetes patients within the community especially with T2DM in Leicester. Their team assistspeople with T2D to manage their diet by designing of nutritional plans, medication, exercise, as well psychological interventions(Leicestershire Diabetes, 2015). ICDS provide training, education, as well as support interventions for “safe management” of “T2D” with “insulin injections”. Currently there with presence of8 clinics in “Leicester” for this delivery of service. These clinics decrease rate of admissions in the hospital by 25%.
There is also “DESMOND program” in Leicester for people with newly diagnosed diabetes and people with established diabetes. The “DESMOND program” offers information about T2D which helps patients to make informed decisions is regards to their treatment as well as in devising care plans.
5.1 Gaps prevalent in services &inequalities provisioning
There is seenvaried gaps as well as inequalities in the provision of community services for “T2D in Leicester” as patients diagnosed with “complex care needs” in “T2D” are not eligible for opting for“ICDS”.There is inadequacy in space for “T2D” self-management programs, also community diabetes specialist services have been recognised to be sparse as well as uncoordinated. There are varied population suffering from T2D, that are vulnerable such as individuals with mental health problems, learning disabilities, asylum seekers,andrefugees, who might not be able to access these servicesavailable.A major backdrop of the “DESMOND program in Leicester” is that it is not delivered in any of the language spoken in African (Desmond, 2019).Moreover, individuals from hugeSomalian community in Leicester might not at all be able to access the service due to prevalence of language barriers. Another major barrier in these community services is that the disabled, old, and housebound patients might not be able to reach these services to access them.
5.2 Working of multi-Agency
The working of multi-agency is essential in managing of LTC and needs collaborating between agencies so as to provide high quality care for the patients. The NHS plan(2000) has a target of dropping health inequalities of individualsfrom BME backgrounds while lowering of gaps in services especially in the deprived areas. The plan also initiates theredeploymentof resourceswithin primary care for the management of inequalities (NHS, 2000) About “T2D”, it was reviewed the NHS plan and then gave birth to the “NSF for diabetes” whose goals are to reduce inequalities and improve service provision in the community (The British Diabetic Association, 2020). NHS England improves quality outcomes for diabetes through CCGs who provide excellent quality care for diabetes.
Voluntary agencies such as“Diabetes UK” and “Leicestershire diabetes” provides interventions for the management of diabetes in Leicester. “Diabetes UK” provides self-help information regarding management of diabetes also providing lifestyle advice.“Leicestershire Diabetes” provides information to the affected patients through digital platforms. The charities are known to support groups which offer patients a chance for meeting and sharing of experiences with others
Role of carers involves monitoring of blood glucose levels and administering of insulin injections to people who are unable to self -manage. Carers manage medication and personal care for the patients. Multi-professional service provision is therefore essential meeting the needs of patients with LTC and thus forming a collaborative approach between agencies for providing quality care outcomes
6. 0 Health Needs assessment
A Learning disability nurse helps in educating the family about diabetes referring the clients to diabetic nurses thus promoting health lifestyle diet management.
HNA includes the systematically evaluating of the health issues of the population, as it identifies priorities as well as hidden needs. It also helps in assigning resources which assists in reducinginequalities and thereby improving health. The status of HNA includes rendering information to plan, negotiate, and change services for improving health. Maslow’s Hierarchy of Needs is essential in the “HNA” for people suffering from“T2D”. Maslow identified needs that include physiological, love/belonging, safety, self-esteem, and self-actualization needs (Beran, 2014).
6.1 “Physiological Needs”
6.1.1 “Nutrition”
Amongst nutritional needs includes a balanced diet for patients suffering from“T2D” diabetes for managing their “glycaemic levels” and preventing the complications of hyperglycemia and hypoglycemia. Normal levels for blood glucose should be 4-7 mmol/l. Thus, for the patients on oral medication/ insulin, healthy and nutritional diet will assists in reducing the dose while also stabilize glycaemic levels, and decline the risk of blood pressure and heart diseases (Bayoumi, 2012). Nurses will provide dietary advice at diagnosis for enabling patients in making informed choices regarding the quantity and type of food consumed. Patients must be provided with a consultation with a dietitianduring the time of diagnosis
6.1.2 “Maintaining Blood glucose”
Patients suffering from“T2D” tend to have fluctuating levels of blood sugar. En-hancement of blood glucose control is essential to reduce the risk as well as severity of microvascularalong with large vascularcomplications of T2D. Achieving a good blood sugar level depends on how the patient understands the dietary balance check to reach that level. Using a diary, patients can record the intake of food as well as blood glucose results and think about their dietary intake, which will promote good blood glucose control. DSNs provides training and support to detect and monitor blood glucose levels to monitor adequate blood glucose levels and helps patients manage T2D (Morrisse et al, 2019).
6.2 Safety Needs
6.2.1 “Foot Health”
Patients with “T2D” are seen to be at considerable risk of neuropathy caused due to high blood sugar levels. Maintaining the blood sugar levels close to normal is impor-tant to prevent foot problems. During the annual rest period, t2d staff assess their legs. During the annual screening, nurses recommend that patients with changed foot shapes wear professional shoes ororthopedic shoes, while providing patients with effective foot care information as part of preventive care (Bayoumi&Alwakeel, 2012).
6.2.2Safety with insulin injections
Some patients with T2D may require insulin injections, so it is necessary to provide education and support to patients who inject insulin to participate in the treatment and solve all problems and problems (Bodicoat et al., 2015). Insulin injections can affect all aspects of a patient's lifestyle, such as intravenous injections and treatment. Nurses regularly inspect the injection site and urge patients to delay lipid nutrition prevention.Sharps injuries may happen to the patient. The nurse will provide cleaned binswhilearranging for their disposalforavoiding sharps injuries.
6.3 “Love and Belonging needs”
6.3.1 “Erectile dysfunction”
ED has been seen a common complication amongst males with T2D and the feel-ings about ED as it is considered as taboo discussion. This also acts as a barrier that might prevent screening as some nurses might feel uncomfortable in discussing matters related to ED. ED has been seen to have profound impacts on the sexual lives and relationships of those affected (Dunkley et al, 2017).
6.4 “Self-Esteem needs”
6.4.1 “Depression”
Depression is very common in people with T2D. Depression is seen to lead to poor dedication towards medication and poor glycaemic monitoring. Depression causes negative behaviors like poor diet and alcoholism which impacts adversely on the management of T2D. Annual depression screening for patients with T2D has be-come an important aspect of the QOF.
6.5 Self-Actualisation
Maslow identified the stage of self-actualisation to be the final stage which an indi-vidual attains. Nurses will be able to educate, empower and support patients with T2D.
Communicating with patients and understanding their values is important in helping the patients to manage their long term conditions. Through communicating and developing a good relationship with the patient the nurse will identify personal values of the patient and thereby support the patient to self-actualize (O'Donovan et al, 2017).
7.0 Conclusion
In conclusion, the current scope of analysis has analysed the definition of diabetes while considering the demographic profile of “Leicester and England”. The gaps as well as inequalities in service provision for T2D have been identified. The report has critically examined the HN of peopledetected with T2D. Thus, it can be said that The increasing prevalence of T2D is a health problem for both Leicester and England. There are currently available several lifestyle services for individuals who are obese in Leicester however the demand for such services is greater than the currently available services. The “Clinics for ICDS” has been seen limited but not assessable by everyone. Some of the BME groups are seen not well represented in the “DESMOND Programme” in Leicester. It is a recommendation increase in the number of spaces in the “DESMOND Program” for T2D patients. Leicester has a large Somalian community and the “DESMOND program” should be provided in their language forovercoming the linguistics barrier that further restricts access to the services. The number of clinics of“ICDS”need to be increased for meeting the needs as well as demand of patients.
8.0 Reference List
Bayoumi, M., and Alwakeel, J., 2012.Hemodialysispatients needs priorities according to maslows hierarchy and quality of life. Journal of Palliative Care & Medicine, 2(2), p.43.
Bayoumi, M., 2012.Identification of the needs of haemodialysis patients using the concept of Maslow's hierarchy of needs. Journal of renal care, 38(1), pp.43-49.
Beran, D., 2014. Developing a hierarchy of needs for Type 1 diabetes. Diabetic Medicine, 31(1), pp.61-67.
Bergman, M., 2013.Pathophysiology of prediabetes and treatment implications for the prevention of “Type 2 Diabetes”mellitus. Endocrine, 43(3), pp.504-513.
Bodicoat, D.H., Carter, P., Comber, A., Edwardson, C., Gray, L.J., Hill, S., Webb, D., Yates, T., Davies, M.J. and Khunti, K., 2015. Is the number of fast-food outlets in the neighbourhood related to screen-detected “Type 2 Diabetes”mellitus and associated risk factors?. Public health nutrition, 18(9), pp.1698-1705.
Cities Changing Diabetes, 2018 Leicester joins cities changing diabetes. [online] Available at:
Desmond, 2019.What is the DESMOND Programme? [online] Available at:
Diabetes”and glucose intolerance in a population with intellectual disabilities: the STOP diabetes cross?sectional screening study.Nursing assignment Journal of intellectual disability research, 61(7), pp.668-681.
Leicester City Council, 2015.Indices of Deprivation. [online] Available at:
Leicester Government UK, 2015. Population and CYP in Leicester. [online] Avail-able at:
Mostafa, S.A., Davies, M.J., Webb, D.R., Srinivasan, B.T., Gray, L.J. and Khunti, K., 2012.Independent effect of ethnicity on glycemia in South Asians and white Europeans. Diabetes Care, 35(8), pp.1746-1748.
NHS, 2017.Diabetes. [online] Available at:
NHS, 2020.What is type 2 diabetes? [online] Available at:
The British Diabetic Association, 2020.Diabetes Prevalence 2019. [online] Available at:
The British Diabetic Association, n.d.Tackling the crisis: Transforming diabetes care for a better future England. [online] Available at: